Chronic Obstructive Pulmonary Disease (COPD)
What is COPD?
According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease 2024 report3, Chronic Obstructive Pulmonary Disease (COPD) is defined as “a heterogeneous lung condition characterized by chronic respiratory symptoms (dyspnea, cough, sputum production and/or exacerbations) due to abnormalities of the airways (bronchitis, bronchiolitis) and/or alveoli (emphysema) that cause persistent, often progressive, airflow obstruction.”
COPD is a common, preventable and treatable disease, the result of long-term exposure and inhalation of harmful substances.
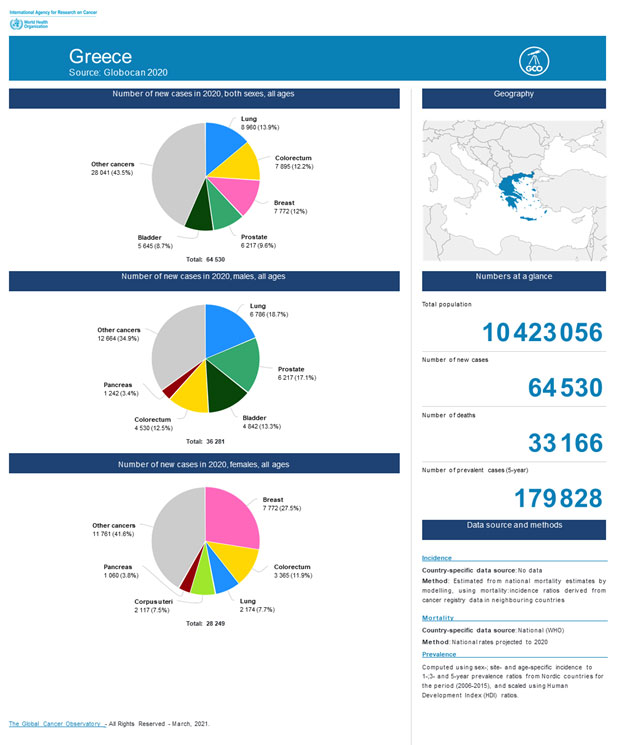
Globally1,
- Currently there are 300 million individuals suffering from COPD
- COPD is the 3rd leading cause of mortality
Risk Factors
Tobacco Smoke
- 90% of cases of COPD are caused by smoking. Tobacco smoke contains irritative, toxic and carcinogenic substances. Non-smokers who are passively exposed to tobacco smoke also have an increased risk for developing COPD.
- Water-pipe, cigars, pipes, roll your own cigarettes and marijuana are also risk factors
Factors during gestation period and childhood
In childhood, important risk factors for developing COPD later in life are:
- Exposure to maternal smoking in utero or in childhood
- Frequent respiratory infections
- Asthma and bronchial hyper-reactivity
Environmental Factors
- Pollution: harmful substances in the air and indoor air contribute to the onset, exacerbation and worsening of the disease.
- Occupational exposure to harmful substances for example working in mining, agriculture or food processing.
Genetic Factors
- Alpha-1 Antitrypsin Deficiency (AATD), a hereditary condition, represents a genetic risk factor for COPD Symptoms
Symptoms
Manifestations of COPD are subtle and gradual worsens over time. In the early stages, it is characterized by a persistent cough (sometimes referred to as ‘smokers cough’) with or without production of phlegm. In addition, other common symptoms are:
- Chronic cough
- Excess phlegm production especially during exacerbations most commonly caused by respiratory infections
- Wheeze (whistling sound) when breathing normally
- Difficulty taking a deep breath
- Shortness of breath, initially upon exertion which worsens over time when doing even minimal tasks or at rest.
- Shortness of breath, initially upon exertion which worsens over time when doing even minimal tasks or at rest.
Exacerbations of COPD are episodes of increased severity of symptoms, most commonly triggered by respiratory infections such as the seasonal flu. Exacerbations accelerate the decline in lung function and worsen the condition.
Individuals with COPD are considered a vulnerable population, at high risk for complications and death from influenza infection, pneumonia, surgery etc.
COPD & COVID-19 pandemic:
COPD is associated with an increased risk for more severe COVID-19 manifestations and poor outcome, although it is not considered a risk factor for acquiring COVID-19 more easily than the general population (Simons et al. Caring for patients with COPD and COVID-19: a viewpoint to spark discussion. Thorax.. December 2020 Vol 75 No 12).
Diagnosis
- Medical and smoking history and physical examination
- Spirometry testing: a non-invasive test widely used to identify and measure the characteristic air flow limitation of the disease. Therefore, spirometry is used in routine clinical practice for:
- Diagnosing COPD
- Staging disease severity
- Pre-operative evaluation
- Monitoring exacerbations
- Evaluating response to treatment
Treatment
COPD requires close monitoring by a pulmonologist who will evaluate your symptoms, complaints and Spirometry, will determine disease severity, as well as identify possible comorbidities, in order to provide the best treatment options for you. This includes quitting smoking and one or more of the following treatments:
- Medications such as inhaled bronchodilators and corticosteroids
- Antibiotics
- Oxygen therapy
- Physiotherapy and respiratory rehabilitation therapies for
- sputum elimination and increasing exercise tolerance
- Proper management of comorbidities
- Addressing depression and social isolation
Prevention
- The most effective measure to prevent COPD is to never smoke, while it is strongly recommended for smokers to quit.
- Avoiding passive exposure to second-hand smoke especially during pregnancy/gestation, childhood and adolescence since it damages the lungs that are still under development.
- Smokers are at high risk for COPD while many smokers in Greece are unaware that they have COPD. Therefore, smokers, especially those with “smoker’s cough”, warrant a spirometry test and a visit to their pulmonologist for early prevention
Secondary prevention (among those who have COPD) aims at reducing the frequency and severity of exacerbations by:
- Quitting smoking of cigarettes, roll-your own cigarettes, water-pipe, pipe, cigars and marijuana
- Getting the seasonal Flu vaccine and Pneumococcal vaccine
- Avoiding second-hand smoke • Avoiding exposure to other toxicants at work or at home
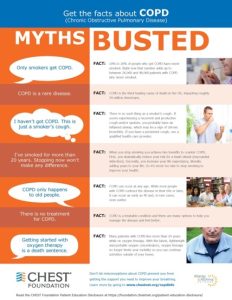
The Chest Foundation has published a facts sheet presenting common myths for COPD2
ANNA S. TZORTZI MD, FCCP
PNEUMONOLOGIST
References
1. Forum of International Respiratory Societies https://www.firsnet.org/news-and-events/news-article/154-world-copd-day-2020
2. CHEST Foundation https://foundation.chestnet.org/wp-content/uploads/2020/05/COPD-Mythbuster.pdf
3. GLOBAL INITIATIVE FOR CHRONIC OBSTRUCTIVE LUNG DISEASE GLOBAL STRATEGY FOR THE DIAGNOSIS, MANAGEMENT, AND PREVENTION OF CHRONIC OBSTRUCTIVE PULMONARY DISEASE (2024 REPORT) https://goldcopd.org/